Obesity is considered to be the primary preventable risk factor for osteoarthritis, and being overweight or obese significantly increases the chances of getting osteoarthritis in the knee, hip, and even in the hand. Relatively small levels of weight loss have been associated with decreased pain. However, the mechanisms linking osteoarthritis and obesity are not well understood. In a 10-year NIH program project grant, The laboratory and an interdisciplinary team of investigators have studied how metabolic factors interact with the altered mechanical loading in obesity. In clinical studies, the team has been studying the effects of weight loss, dietary content, exercise, on knee pain, and together have developed new physical and psychological therapies that are being used clinically to help people cope better with osteoarthritis. Most recently, work in the laboratory has shown that the severity of obesity and injury-induced osteoarthritis is highly dependent on diet as well as weight gain. Taken together, these studies provide increasing evidence for the role of inflammation, due to dietary content or systemic inflammation, acting in concert with abnormal mechanical, in the onset and progression of obesity-induced osteoarthritis.
Mechanical factors play a critical role in regulating the metabolic response of chondrocytes in both health and disease. A significant thrust of the laboratory has been to combine theoretical modeling and experimental studies to investigate the micromechanical environment of chondrocytes and its role in regulating chondrocyte mechanotransduction. These studies have led to the identification of several ion channels, such as Transient Receptor Potential Vanilloid 4 (TRPV4) and Piezo1&2, as a critical sensors of mechanical and osmotic loading in chondrocytes. Subsequently, the laboratory has developed a library of novel small molecule compounds to modulate and tune the activity of the channel as a therapeutic approach for osteoarthritis and as an alternative approach to artificially simulate “bioreactor” loading for accelerating tissue formation in engineered cartilage.
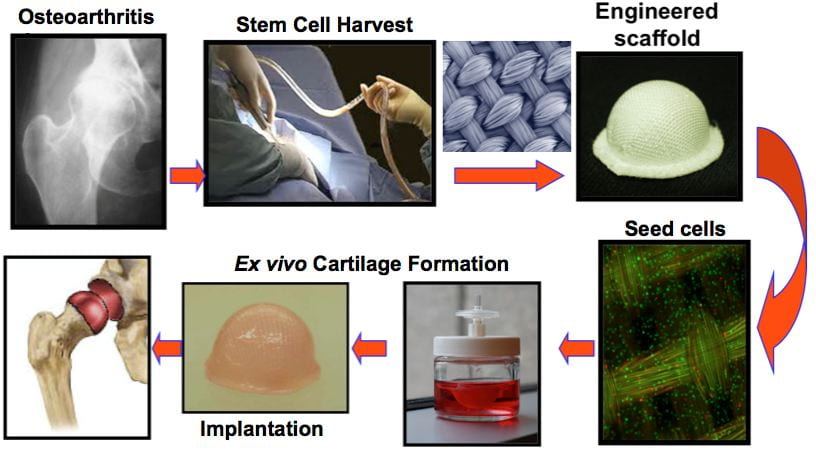
The primary surgical treatment option currently available for patients with end-stage osteoarthritis is total joint replacement with a metal and plastic prosthesis. While this is an excellent procedure and generally provides significant pain relief, joint replacements typically last only about 15 years, and revision surgeries are prone to complications. A major thrust in the laboratory is the development of new stem cell-based approaches to treat osteoarthritis. His lab developed a technique to weave biodegradable fibers in 3D to create an exact template of the joint surface as a scaffold for these cells. Other projects are examining how the inflammatory environment within an injured or diseased joint could actually prevent the process of repair or regeneration, focusing on developing new anti-inflammatory approaches based on purified stem cell injections or combined gene-therapy and tissue-engineering to enhance joint repair. Most recently, his work as focused on genome editing and synthetic biology, using techniques such as the CRISPR/Cas9 system to create custom-designed cells for regenerative medicine and drug screening for osteoarthritis.